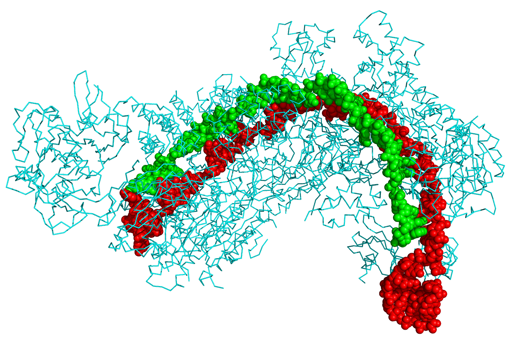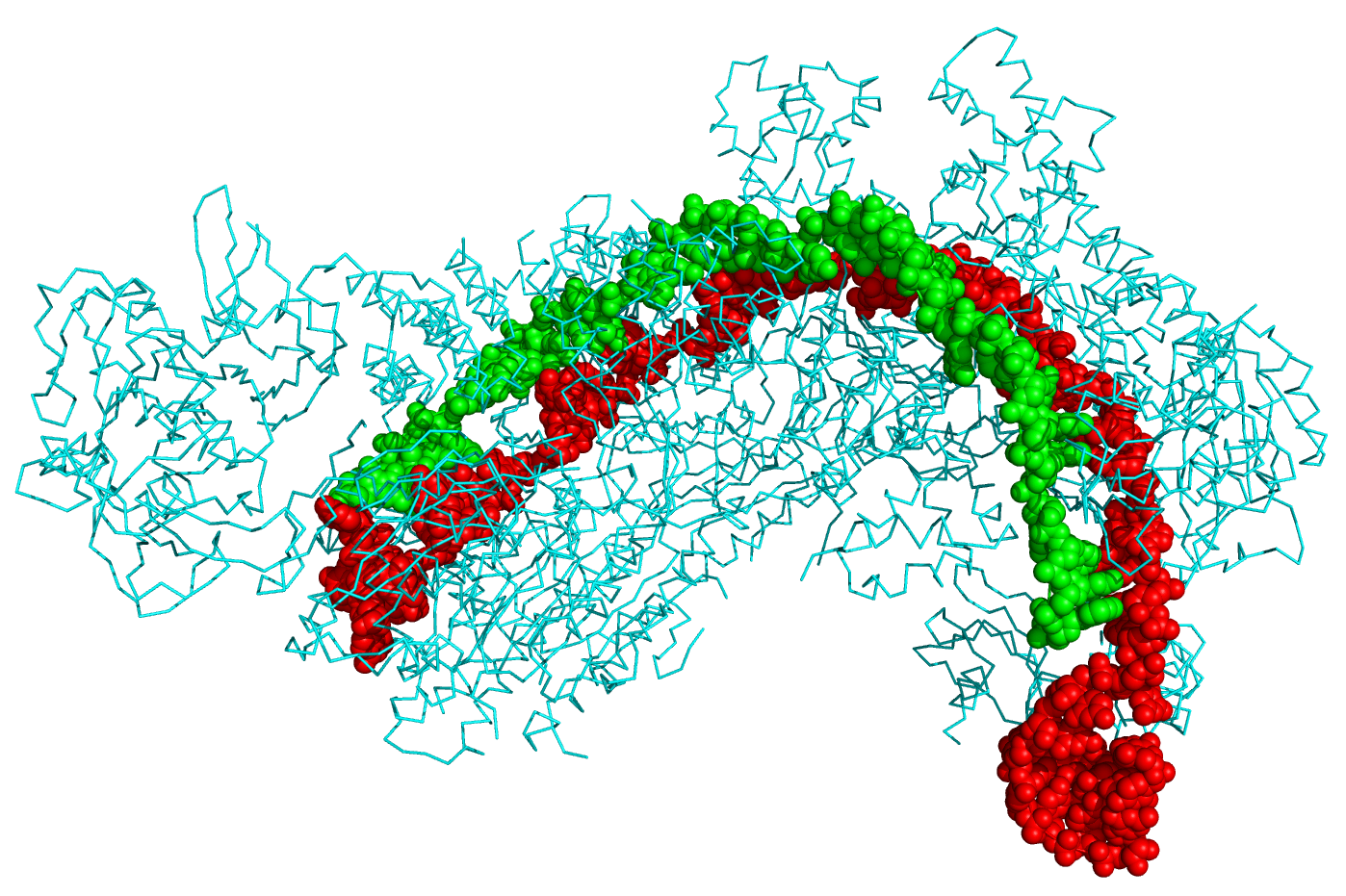
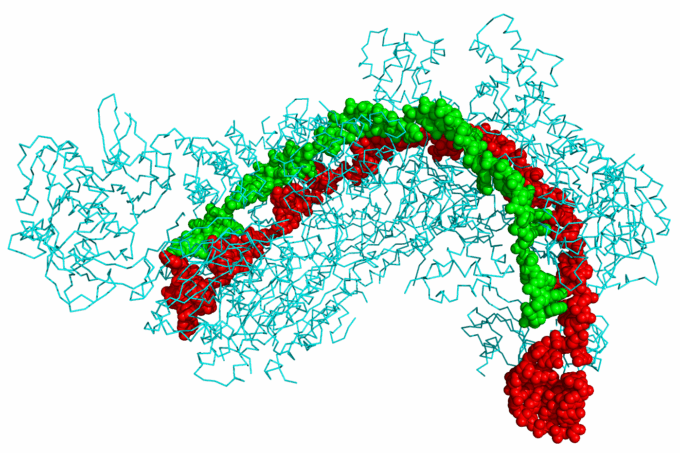
Crystal structure of a CRISPR RNA-guided surveillance complex. Image Source: Boghog – CC BY-SA 4.0
A major medical milestone took place in May 2025, when doctors at the Children’s Hospital of Philadelphia used CRISPR-based gene editing to treat a child with a rare genetic disorder. Unlike earlier CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats) treatments that targeted well-known genetic mutations, this marked a new level of personalized medicine tailored to a patient’s unique DNA. For advocates of biomedical innovation for human enhancement, it was another sign of gene editing’s vast potential, even as ethical, political, and safety concerns remain.
Efforts to alter human genes really began in the 1970s, when scientists first learned to cut a piece of DNA from one organism and attach it to another. The process was slow, imprecise, and expensive. Later tools like meganucleases, transcription activator-like effector nucleases, and zinc-finger nucleases improved accuracy but remained technically complex and time-consuming.
The real revolution came in 2012, when researchers Jennifer Doudna and Emmanuelle Charpentier harnessed CRISPR, a natural bacterial defense system. In bacteria, CRISPR cuts out invading viruses’ DNA and inserts fragments into its own genome, allowing it to recognize and defend against future infections. Doudna and Charpentier showed that this process could be adapted to any DNA, including human, creating a precise and programmable system to target genetic mutations. Together with a protein called CRISPR-associated protein (Cas9), which acts like molecular scissors, it made cutting, modifying, and replacing DNA faster, easier, and cheaper.
Attempts to push the technology forward clashed with regulatory caution and ethical debate, but more than 200 people had undergone experimental CRISPR therapies, according to a 2023 MIT Technology Review article. The first major legal breakthrough came that November, when the UK approvedVertex Pharmaceuticals’ CASGEVY for the treatment of transfusion-dependent beta thalassemia and sickle cell disease. Enabled by advances in CRISPR technology, CASGEVY works by making “an edit (or ‘cut’)… in a particular gene to reactivate the production of fetal hemoglobin, which dilutes the faulty red blood cells caused by sickle cell disease,” explained Yale Medicine. Bahrain and the U.S. granted regulatory approval weeks later, and by mid-2025, the EU and several other countries followed.
CRISPR technology continues to advance, with researchers at the University of Texas at Austin recently unveiling a CRISPR therapy that can replace large defective DNA segments and fix multiple mutations simultaneously, overcoming the limits of traditional one-site editing. “Epigenetic editing,” meanwhile, uses modified Cas9 proteins to turn genes on or off without cutting the DNA, and new CRISPR systems can even insert entirely new DNA directly into cells, bypassing the cell’s natural repair process for larger precision edits.
Alongside academic researchers, major companies are emerging in the gene-editing field. By early 2025, the U.S. had 217 gene-editing companies, compared with a few dozen in Europe (mainly in the UK and Germany) and 30 in China, according to the startup company BiopharmaIQ.
CRISPR Therapeutics, Intellia Therapeutics, and Beam Therapeutics are among the industry’s leaders. A growing network of companies and research teams attended the Third International Summit on Human Genome Editing held in London in 2023, following the first in Washington, D.C., in 2015, and the second in Hong Kong in 2018.
Smaller companies are also innovating. Xenotransplantation—transplanting nonhuman organs to humans—has a long history, but CRISPR technology is giving it new momentum. In 2024, Massachusetts General Hospital transplanted a pig kidney edited with CRISPR-Cas9 technology to remove harmful pig genes and add human ones. The pig kidney was provided by the American pharmaceutical company eGenesis.
The patient survived for two months before dying of unrelated causes, and the company completed another transplant in 2025. Other companies, including United Therapeutics through its subsidiary Revivicor, have begun their own trials in a potential bid to transform the organ donor industry.
CRISPR’s rapid spread has also fueled a DIY biotech movement among transhumanists and biohackers interested in using biotechnology for human enhancement. Nonconventional genetic experimentation, or “garage research,” often outside standard regulation, has become common. CRISPR kits can be ordered online for less than $100, and their small size, relative simplicity, and open-source nature make experimentation and collaboration possible.
“[N]ew technologies such as CRISPR/Cas9 give nonconventional experimenters more extensive gene editing abilities and are raising questions about whether the current largely laissez-faire governance approach is adequate,” pointed out a 2023 article in the Journal of Law and the Biosciences.
One of the best-known figures in this movement is former NASA biochemist Josiah Zayner, who founded The ODIN in 2013 to sell CRISPR kits “to help humans genetically modify themselves.” Early efforts to showcase the scope and potential of this technology proved popular online, and in 2017, Zayner livestreamed injecting CRISPR-edited DNA to knock out his myostatin gene to promote muscle growth.
[Content truncated due to length…]
From CounterPunch.org via this RSS feed